TB-500 Tβ4
Thymosin Beta-4 (Tβ4) is a naturally occurring 43-amino-acid peptide found in nearly all human tissues and is a key mediator of tissue repair, regeneration, and protection. It promotes wound healing, angiogenesis, inflammation modulation, and scar reduction by binding actin and enhancing cell migration. TB-500 is the synthetic research version of the full-length Tβ4 peptide, developed for stability and consistency in experimental use. TB-500 Fragment (17-23) is a smaller bioactive sequence of the parent peptide that replicates many of Tβ4’s regenerative effects—particularly actin binding and wound repair—while being shorter in length and sometimes more cost-effective for targeted studies. Together, these compounds provide valuable models for studying tissue regeneration, cardiovascular repair, and cellular protection in laboratory settings.
$89.99
In stock
Disclaimer: This compound is not intended for human or veterinary use. TB-500 (Tβ4) is sold strictly for laboratory research purposes only. Any mention of effects is provided for educational information and relates solely to preclinical or experimental studies and does not imply efficacy in humans.
Wound Healing & Tissue Regeneration
- Promotes rapid re-epithelialization and wound closure in skin, corneal, and internal injury models.
- Enhances keratinocyte, fibroblast, and endothelial migration into damaged tissue.
- Stimulates progenitor cell activation for regeneration in cardiac, dermal, and neural models.
- Supports recovery of tissues in compromised healing conditions (e.g., diabetes, aged animals).
Angiogenesis & Microvascular Recovery
- Upregulates VEGF and stabilizes HIF-1α, stimulating robust new blood vessel growth.
- Activates PI3K/Akt/eNOS signaling, increasing nitric oxide and endothelial function.
- Increases capillary density and perfusion in ischemic or injured tissues.
- Demonstrated enhanced neovascularization in wound, ocular, and cardiac repair models.
Inflammation Modulation & Cytoprotection
- Suppresses NF-κB signaling, reducing pro-inflammatory cytokines (e.g., TNF-α, IL-6).
- Decreases immune cell infiltration into injured tissue, shortening inflammatory phase.
- Protects cells from apoptosis via caspase inhibition and Bcl-2 upregulation.
- Reduces oxidative tissue injury and improves survival in ischemia/reperfusion models.
Cellular Migration & Stem Cell Recruitment
- Acts as the major G-actin–sequestering protein, enabling cytoskeletal remodeling and cell motility.
- Increases endothelial, epithelial, and repair cell migration into wound sites.
- Mobilizes epicardial progenitors and endothelial progenitor cells in cardiac regeneration.
- Enhances stem/progenitor cell homing and differentiation in dermal, cardiac, and neural systems.
Fibrosis Reduction & Scar Remodeling
- Inhibits TGF-β/Smad signaling, reducing myofibroblast activation.
- Limits collagen over-deposition, resulting in reduced fibrotic scarring.
- Encourages regenerative (scarless) healing instead of fibrotic repair.
- Demonstrated anti-fibrotic effects in cardiac, hepatic, renal, and pulmonary models.
Muscle, Cardiac & Connective Tissue Regeneration
- Preserves cardiomyocytes post-infarction and activates cardiac progenitors for repair.
- Stimulates myogenesis and supports functional recovery in muscle regeneration models.
- Improves tendon, ligament, and corneal repair in preclinical studies.
- Frequently paired with IGF-1, MGF, or BPC-157 for synergistic repair in musculoskeletal and cardiovascular research.
Neuroprotection & Ocular Regeneration
- Enhances neuronal survival by reducing apoptosis in ischemic and traumatic brain injury models.
- Stimulates oligodendrocyte progenitor differentiation and myelin repair in neuroregeneration studies.
- Promotes corneal wound healing and dry eye recovery, reducing inflammation and scarring.
- Demonstrated both preclinical and clinical efficacy in ocular surface disorders (e.g., neurotrophic keratopathy, dry eye).
To maximize the regenerative potential of Thymosin Beta-4 (Tβ4) in experimental models, researchers often combine it with complementary compounds that enhance angiogenesis, anti-fibrosis, progenitor activation, or immune modulation. These synergies have been explored in dermal repair, cardiac recovery, neuroprotection, and ocular regeneration models.
Tβ4 Synergistic Compounds
| Compound | Mechanism of Synergy | Relevant Research / Notes |
|---|---|---|
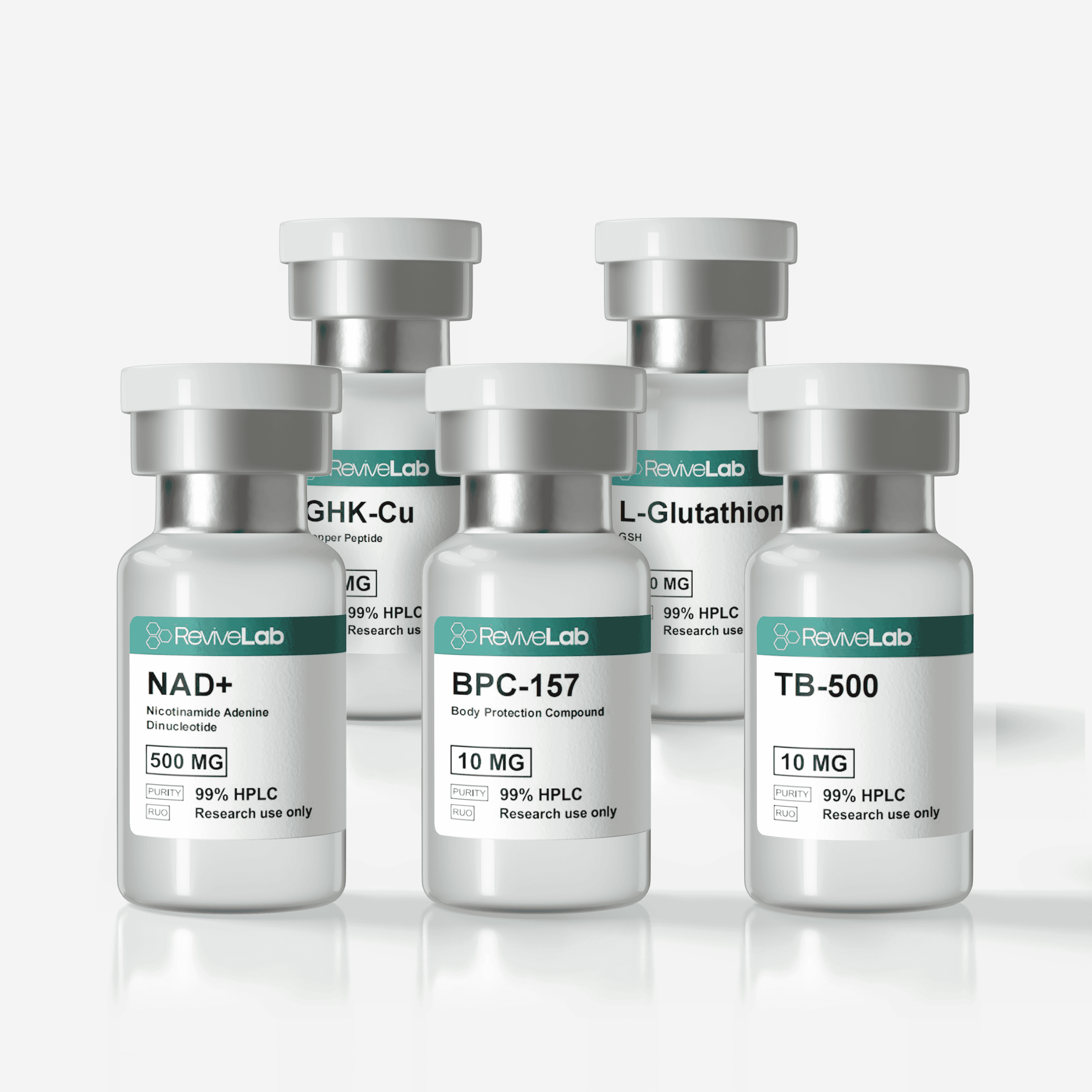
| BPC-157 | Promotes angiogenesis, tendon/ligament repair, and fibroblast migration; complements Tβ4’s actin-binding and wound closure pathways. | Chang et al., 2014 – Enhanced tendon healing via GH receptor modulation; pairs with Tβ4 to accelerate connective tissue repair. |
| GHK-Cu | Stimulates collagen synthesis, ECM remodeling, and skin rejuvenation; synergizes with Tβ4’s anti-fibrotic effects. | Studies in dermal wound and cosmetic models show improved scar remodeling and epithelial repair with combined use. |
| Thymosin Alpha-1 (Tα1) | Potent immunomodulator; enhances epithelial repair and endothelial migration; complements Tβ4’s anti-inflammatory pathways. | Malinda et al., 1999 – Tα1 promoted endothelial migration; combining with Tβ4 supports tissue regeneration in immune-challenged models. |
| IGF-1 LR3 | Activates muscle satellite cells, stimulates hypertrophy, and supports tissue growth; synergistic with Tβ4 in skeletal and cardiac muscle models. | Godard et al., 2013 – Improved lean mass and recovery; works alongside Tβ4’s progenitor activation for muscle regeneration. |
| MGF (IGF-1Ec) | Local injury-specific IGF isoform that stimulates satellite cell proliferation and localized repair. | Si et al., 2017 – Promoted local muscle fiber repair; combined with Tβ4 enhances muscle recovery models. |
| Glutathione | Potent antioxidant; reduces oxidative stress during tissue repair; complements Tβ4’s cytoprotective and anti-apoptotic functions. | Cardiac ischemia-reperfusion models demonstrate that reducing ROS synergizes with Tβ4’s survival-promoting effects. |
| NAD⁺ | Supports mitochondrial biogenesis and DNA repair; enhances cellular energy for regeneration; pairs with Tβ4’s actin-driven migration. | Preclinical studies indicate improved cell survival and progenitor activity when NAD⁺ restoration accompanies regenerative peptides. |
Potential Research Use Cases for Tβ4 Combinations
- Tendon & Ligament Repair:
Tβ4 + BPC-157
→ Dual-pathway repair via angiogenesis, fibroblast migration, and cytoskeletal remodeling. - Cardiac Regeneration Models:
Tβ4 + IGF-1 LR3 / MGF
→ Supports cardiomyocyte survival, progenitor mobilization, and vascular repair post-infarction. - Dermal Healing & Cosmetic Research:
Tβ4 + GHK-Cu
→ Improves skin regeneration, collagen remodeling, and reduces fibrotic scarring. - Ocular & Corneal Repair:
Tβ4 + Thymosin Alpha-1
→ Combines immune regulation with epithelial migration to accelerate corneal and ocular surface healing. - Neuroprotective & Anti-Oxidative Research:
Tβ4 + Glutathione + NAD⁺
→ Comprehensive support for neuronal survival, reduced oxidative stress, and enhanced energy metabolism in neuroregeneration models. - Post-Surgical & Multi-Tissue Recovery:
Tβ4 + BPC-157 + GHK-Cu
→ Comprehensive regenerative model for wound closure, connective tissue repair, and cosmetic remodeling.
Thymosin beta-4 (Tβ4) is a naturally occurring 43-amino-acid peptide prominent in nearly all human tissues. It is a key mediator of tissue repair, regeneration, and protection. Tβ4 is best known for its ability to bind actin (a major cell structural protein) and promote cell movement, which is crucial for wound healing Malinda et al. (Ref. 1). Research has revealed a wide array of biological functions for Tβ4 – from accelerating wound healing and new blood vessel growth to reducing inflammation and scarring – making it a promising therapeutic peptide in regenerative medicine Goldstein & Kleinman (Ref. 6), Xing et al. (Ref. 10).
Mechanism of Action
Tβ4’s primary mechanism involves G-actin binding: it sequesters actin monomers, modulating the cytoskeleton and thereby enhancing cell migration and tissue remodeling Safer et al., 1991. This action facilitates the movement of cells (including immune cells and fibroblasts) to sites of injury. Additionally, Tβ4 influences multiple cell signaling pathways that govern survival and healing. For example, it upregulates pathways like PI3K/Akt/eNOS (promoting cell survival and angiogenesis) Jo et al. (Ref. 9) and Wnt/β-catenin (involved in hair follicle growth) Philp et al. (Ref. 2), while downregulating NF-κB Qiu et al., 2011 and TGF-β signaling to reduce inflammation and fibrosis Cavasin et al. (Ref. 8). Through these combined mechanisms, Tβ4 orchestrates a comprehensive repair response after injury.
Wound Healing & Tissue Regeneration
Tβ4 plays a vital role in repairing injured tissues and accelerating wound healing. After an injury, Tβ4 is released by platelets and immune cells at the site to protect tissues from further damage and to reduce excessive cell death and inflammation Malinda et al. (Ref. 1). It actively promotes the migration of cells into the wound and the formation of new blood vessels, while also encouraging stem/progenitor cells to differentiate and replace damaged tissue Philp et al. (Ref. 2). Notably, Tβ4 decreases the presence of myofibroblasts (scar-forming cells) in wounds, which leads to less scar tissue and more complete regeneration of normal tissue structure Goldstein & Kleinman (Ref. 6).
Angiogenesis & Improved Blood Flow
Thymosin beta-4 is a potent stimulator of angiogenesis, the growth of new blood vessels. It upregulates vascular endothelial growth factor (VEGF) and other angiogenic factors, resulting in greater capillary formation and blood supply in injured or ischemic tissues Jo et al. (Ref. 9), Xing et al. (Ref. 10). In research models, Tβ4 significantly increased capillary density and blood perfusion – for instance, combining Tβ4 with stem cells in a limb ischemia model led to enhanced blood flow recovery in the affected limb Smart et al. (Ref. 4). By improving microcirculation, Tβ4 helps deliver oxygen and nutrients to regenerating tissues, a critical step in healing.
Anti-Inflammatory & Immune Modulation
Tβ4 has demonstrated strong anti-inflammatory properties. It dampens the production of pro-inflammatory cytokines (such as TNF-α, IL-1β, IL-6) by blocking activation of NF-κB and related inflammatory pathways Qiu et al., 2011. In autoimmune injury models, Tβ4 treatment led to markedly fewer inflammatory cells in affected tissues (e.g. reduced immune cell infiltration in the brain in an MS-like encephalomyelitis model) Xing et al. (Ref. 10). It also protected organs from inflammatory damage in systemic injury models – for example, Tβ4 prevented the surge of inflammatory cytokines in a severe liver injury and alcohol exposure model Shah et al., 2018. Through down-regulating inflammatory chemokines and cytokines, Tβ4 creates a more favorable environment for healing and tissue regeneration Goldstein & Kleinman (Ref. 6). This peptide even exhibits some anti-microbial support, as studies note it can limit microbial growth in wounds and infected tissues, thereby reducing infection-related complications Malinda et al. (Ref. 1).
Anti-Apoptotic (Cell Survival) Effects
Another critical function of Tβ4 is protecting cells from apoptosis (programmed cell death) during stress or injury. It has been shown to increase cell survival by inhibiting key apoptosis mediators. In cellular studies, Tβ4 exposure reduced the activation of caspase-3 and -9 (enzymes that drive apoptosis) and preserved mitochondrial integrity, thereby keeping cells alive under otherwise lethal conditions Sosne et al., 2004. For example, Tβ4 prevented corneal epithelial cells from undergoing apoptosis after ethanol injury in vitro, acting as an anti-apoptotic agent for the eye Sosne et al., 2004. In models of brain ischemia (stroke), Tβ4 upregulated protective chaperone proteins (like GRP78) and anti-death proteins (Bcl-2), while downregulating pro-apoptotic signals, resulting in reduced neuron loss after injury Xing et al. (Ref. 10). By preserving cells from dying, Tβ4 ensures that more of the tissue is retained and able to recover function post-injury.
Antioxidant & Cytoprotective Activity
Tβ4 also exerts antioxidative effects that shield tissues from oxidative stress. Research indicates Tβ4 can increase the scavenging of reactive oxygen species (ROS) in cells, lessening oxidative damage Ho et al., 2008. In models of ischemia-reperfusion injury (where returning blood flow causes oxidative damage in heart or brain), Tβ4 treatment improved outcomes by boosting antioxidant defenses and reducing tissue damage Shah et al., 2018. Notably, Tβ4 upregulates endogenous antioxidant enzymes (like catalase and SOD) in cardiac tissue, helping neutralize harmful free radicals produced during a heart attack Xing et al. (Ref. 10). This antioxidant property, coupled with its anti-inflammatory and anti-apoptotic actions, makes Tβ4 a powerful cytoprotective agent, protecting cells from diverse forms of injury (even including toxicity from glutamate in neurons) Goldstein & Kleinman (Ref. 6).
Anti-Fibrotic Properties (Reduced Scarring)
Thymosin beta-4 helps prevent excessive fibrosis – the formation of dense scar tissue that can impair organ function. By modulating the TGF-β/Smad signaling pathway, Tβ4 interferes with one of the central drivers of fibrotic tissue formation Cavasin et al. (Ref. 8). The result is a reduction in collagen deposition and scar buildup in healing tissues. Studies have shown that Tβ4 treatment leads to smaller scars and less fibrosis after injuries. In skin wounds, as mentioned, Tβ4 lowers myofibroblast numbers and hence minimizes scar formation Malinda et al. (Ref. 1). In internal organs, Tβ4 has demonstrated anti-fibrotic effects across the board – it reduced fibrous tissue development in models of heart damage, lung injury, liver fibrosis, and kidney disease Xing et al. (Ref. 10). For example, in a heart attack model, Tβ4 not only improved cardiac function but also significantly attenuated cardiac fibrosis, leading to a smaller scar in the heart muscle Smart et al. (Ref. 4).
Stem Cell Recruitment & Differentiation
A remarkable aspect of Tβ4’s regenerative action is its ability to mobilize stem and progenitor cells. Tβ4 essentially “calls in” the body’s repair cells to the site of injury. It has been observed to stimulate the mobilization, migration, and even differentiation of stem cells involved in tissue repair Philp et al. (Ref. 2), Xing et al. (Ref. 10). For instance, Tβ4 enhances the activity of endothelial progenitor cells (EPCs), which form new blood vessels; EPCs pre-treated with Tβ4 showed better survival and integration when transplanted into injured heart tissue, leading to greater repair than EPCs alone Bock-Marquette et al. (Ref. 3), Smart et al. (Ref. 4). In the heart, Tβ4 not only recruits native cardiac progenitor cells but also promotes them to proliferate and mature into new heart muscle cells and blood vessel cells, contributing to regeneration of the damaged heart Smart et al. (Ref. 4). Tβ4 similarly boosts proliferation of other stem cell types (mesenchymal stem cells, neural progenitors, oligodendrocyte precursors), thereby aiding regeneration in various tissues Xing et al. (Ref. 10). By acting as a signal for stem cells to home to injuries and replace lost cells, Tβ4 greatly amplifies the body’s natural healing capacity.
Cardiovascular Repair and Protection
Tβ4 has been extensively studied for its cardioprotective effects. In the event of a myocardial infarction (heart attack), Tβ4 helps preserve heart muscle and improve recovery. It works in two phases: an acute phase immediately after injury (where Tβ4’s anti-apoptotic and anti-inflammatory actions protect the heart muscle at risk) and a chronic phase (where Tβ4 stimulates new blood vessel growth and activates cardiac progenitor cells for heart tissue regeneration) Bock-Marquette et al. (Ref. 3), Smart et al. (Ref. 4). Animal studies have shown that administering Tβ4 after a heart attack can reduce the infarct size (area of dead tissue) and enhance the heart’s contractile function during recovery Smart et al. (Ref. 4). In fact, Tβ4 is one of the first molecules identified that can re-initiate an embryonic-like coronary development program in adult mammalian hearts, essentially encouraging the heart to heal itself in ways normally only seen in embryos Goldstein & Kleinman (Ref. 6), Xing et al. (Ref. 10). Early clinical trials have been promising as well: a Phase II trial in heart attack patients found that Tβ4 treatment was associated with smaller scar formation and improved cardiac function post-infarction, with no serious adverse events reported Pipes et al., 2016. Beyond heart attacks, Tβ4 has been shown to protect heart tissue from ischemia-reperfusion injury and even to improve outcomes in heart transplant models by reducing rejection and boosting blood vessel density in the graft Xing et al. (Ref. 10).
Neuroprotective & Neuroregenerative Effects
Emerging research indicates that Tβ4 benefits the nervous system by protecting neural cells and promoting regeneration. Tβ4 is naturally present in the brain and upregulated after injuries like stroke or trauma, suggesting a role in the brain’s repair processes Goldstein & Kleinman (Ref. 6), Xing et al. (Ref. 10). Experimentally, Tβ4 has been found to induce neurogenesis – for example, infusion of a Tβ4 fragment into the hippocampus spurred the growth of new neurons in adult mice Xing et al. (Ref. 10). It also supports glial cells; Tβ4 enhances the proliferation and maturation of oligodendrocyte progenitor cells, leading to increased formation of myelin (the protective coating on nerves) Xing et al. (Ref. 10). In models of brain injury (ischemic stroke), Tβ4 treatment reduced neuronal cell death by suppressing apoptosis pathways and improved neurological recovery after the insult Xing et al. (Ref. 10). Its anti-inflammatory effect in the central nervous system was demonstrated by decreased microglial activation and inflammatory cytokines in a mouse model of multiple sclerosis when treated with Tβ4 Xing et al. (Ref. 10).
Ocular Healing (Cornea and Dry Eye)
Thymosin beta-4 has shown significant therapeutic potential in the eye, particularly for corneal injuries and dry eye syndrome. In various corneal wound models (chemical burns, mechanical injuries), Tβ4 application led to faster and more complete healing of the cornea Sosne et al. (Ref. 5). It does so by promoting corneal re-epithelialization (helping the cornea’s surface cells migrate and cover the wound) and by moderating the wound environment – Tβ4 reduces harmful inflammation and balances the activity of matrix-degrading enzymes, preventing excessive tissue breakdown Sosne et al. (Ref. 5). Treated corneas had less inflammatory cell infiltration and a better restoration of clarity and structure compared to controls Sosne et al. (Ref. 5). In addition, Tβ4 protects corneal cells from apoptosis and oxidative damage, contributing to tissue survival and regeneration in the eye Ho et al., 2008. Importantly, clinical trials with Tβ4 eye drops in humans have reported improvements in signs and symptoms of moderate-to-severe dry eye disease, with the treated patients experiencing relief that persisted even after the treatment period Sosne et al. (Ref. 7). These trials also noted no significant adverse effects, underlining Tβ4’s safety and efficacy in ocular applications Sosne et al. (Ref. 7). Tβ4 is thus being pursued as a novel treatment for corneal injuries (e.g. persistent corneal ulcers) and dry eye, where it could accelerate healing and reduce inflammation better than standard therapies.
Hair Growth Stimulation
An intriguing function of Tβ4 is its ability to stimulate hair growth. This was initially discovered incidentally – researchers observed that wounds treated with Tβ4 not only healed faster but also grew hair more rapidly around the wound edges Philp et al. (Ref. 2). Subsequent studies confirmed that Tβ4 promotes hair follicle development and cycling. In mouse experiments, animals genetically overexpressing Tβ4 in their skin grew hair back significantly faster after hair removal, and they developed a higher number of new hair shafts and follicles, whereas mice lacking Tβ4 showed delayed and reduced hair growth Dai et al., 2021. Tβ4 appears to activate certain pathways (such as Wnt/β-catenin and MAPK/ERK) and increase growth factors like VEGF in the skin, which together stimulate the hair follicle stem cells and the formation of new hair strands Philp et al. (Ref. 2), Xing et al. (Ref. 10). These effects suggest potential research applications of Tβ4 in conditions like alopecia (hair loss) or for enhancing hair regeneration. Indeed, one study noted that even in vitro hair organ cultures (whisker follicles) showed accelerated growth when exposed to Tβ4 Philp et al. (Ref. 2). While more research is needed to translate this to clinical use, Tβ4’s hair growth-promoting activity adds to its profile as a regenerative peptide.
| Ref. No. | Study / Source | Focus / Key Findings | Link |
|---|---|---|---|
| 1 | Malinda, K.M., et al. (1999). Thymosin β4 accelerates wound healing. | Demonstrated accelerated dermal healing via increased angiogenesis, keratinocyte migration, and collagen deposition. | PubMed |
| 2 | Philp, D., et al. (2004). Thymosin β4 promotes wound repair. | Showed that Tβ4 enhances angiogenesis, dermal repair, and hair follicle development, especially in aged animals. | PubMed |
| 3 | Bock-Marquette, I., et al. (2004). Thymosin β4 activates integrin-linked kinase and promotes cardiac cell migration. | Identified ILK/Akt signaling as the pathway by which Tβ4 improves cardiomyocyte survival and heart repair. | Nature |
| 4 | Smart, N., et al. (2007). Thymosin β4 induces adult epicardial progenitor mobilization and neovascularization. | Demonstrated Tβ4’s role in stimulating progenitor differentiation for cardiac regeneration. | PubMed |
| 5 | Sosne, G., et al. (2007). Thymosin β4 promotes corneal wound healing and reduces inflammation. | Highlighted Tβ4’s protective and anti-apoptotic actions in ocular models. | PMC |
| 6 | Goldstein, A.L., & Kleinman, H.K. (2015). Thymosin β4: a wound healing and regenerative peptide. | Review summarizing Tβ4’s effects on angiogenesis, inflammation modulation, and tissue regeneration. | PubMed |
| 7 | Sosne, G., et al. (2015). Randomized trial of thymosin β4 eye drops for dry eye syndrome. | Clinical evidence of symptom relief and epithelial repair in ocular surface disease. | PubMed |
| 8 | Cavasin MA, Rhaleb NE, Yang XP, Carretero OA. (2004). “Prolyl oligopeptidase is involved in release of the antifibrotic peptide Ac-SDKP.” | Demonstrated that prolyl oligopeptidase is responsible for releasing the antifibrotic peptide Ac-SDKP (derived from Tβ4), and that chronic Ac-SDKP treatment decreases cardiac and renal fibrosis and inflammatory cell infiltration in hypertensive rats. | PubMed |
| 9 | Jo JO, et al. (2010). “Thymosin beta4 induces the expression of vascular endothelial growth factor in endothelial cells.” | Identified VEGF-driven angiogenic mechanisms via PI3K/Akt/eNOS signaling in endothelial cells exposed to Tβ4. | ScienceDirect |
| 10 | Xing Y, et al. (2021). “Progress on the function and application of Thymosin β4 in tissue repair and regeneration.” Front Endocrinol | Comprehensive review covering organ protection, fibrosis prevention, neuroprotection, stem-cell recruitment, and regenerative applications of Tβ4. | PMC |
 Semax
Semax  Bacteriostatic Water
Bacteriostatic Water